Pain is a major clinical problem affecting 1 in 5 people in the world and unrelieved pain is a major global healthcare problem. Pain research in Cambridge is truly interdisciplinary, involving researchers across many departments and schools combining behavioural, computational, genetic, electrophysiological and neuroimaging tools to understand pain perception and behaviour in humans. For example, the ADVANTAGE consortium aims to better understand the neural basis visceral pain and guide improvements on how we treat people with visceral diseases. In fact, one in twenty individuals in the UK are disabled by visceral pain arising from conditions such as endometriosis, inflammatory bowel disease and kidney disease. Using a translational and interdisciplinary approach, uniting patient experts, clinical and pre-clinical pain researchers, visceral disease experts, psychologists, engineers and industrial collaborators will maximise the development of novel study tools, drugs and treatments – specifically tailored for visceral pain.
Unexpected extremes of pain
A collaboration between clinicians and scientists based at Cambridge sought to investigate why some mothers report less pain during labour. They found that those in the test group (i.e. women who feel less pain during childbirth) had a higher-than-expected prevalence of a rare variant of the gene KCNG4. It is estimated that approximately 1 in 100 women carry this variant. KCNG4 encodes a protein that forms part of a ‘gate’, controlling the electric signal that flows along our nerve cells. The genetic variant that was found in women who feel less pain during childbirth leads to a ‘defect’ in the formation of the switch on the nerve cells. In fact, this defect acts like a natural epidural, thus, a much greater signal – in other words, stronger contractions during labour – are required to switch it on. This makes it less likely that pain signals can reach the brain. Driven by studying human lived experience and genetics, collaboration with pre-clinical scientists was necessary to determine the mechanism by which the KCNG4 variant produced the “analgesic” effect. The approach of studying individuals who show unexpected extremes of pain experience also may find wider application in other contexts, helping us understand how we experience pain and develop new drugs to treat it.
What Naked mole-rats can teach us about pain?
Work on pain in Cambridge transcends levels, very evident in the work being done in the Naked Mole-Rat Initiative. Naked mole-rats are incredibly unusual and fascinating creatures that alongside many other traits, display an unusual sensitivity to pain, for example, acid does not cause them pain. Many human conditions involving inflammation – such as arthritis – can create localised acidity. Understanding how naked mole-rats do not feel acid could help researchers understand how acid actually cases pain, and develop new drugs to stop it. Naked mole-rat resistance to neurodegenerative diseases and a healthy ageing brain shows how, like our researchers, the naked mole-rat is a model organism that works across research areas.
Could inflatable shape-changing spinal implants help treat severe pain?
Interdisciplinary research is key in pain research. A team of engineers and clinicians at Cambridge has developed an ultra-thin, inflatable device that can be used to treat the most severe forms of pain without the need for invasive surgery. The device, developed by researchers at Cambridge, uses a combination of soft robotic fabrication techniques, ultra-thin electronics and microfluidics. The device is so thin – about the width of a human hair – that it can be rolled up into a tiny cylinder, inserted into a needle, and implanted into the epidural space of the spinal column, the same area where injections are administered to control pain during childbirth. Once correctly positioned, the device is inflated with water or air so that it unrolls like a tiny air mattress, covering a large section of the spinal cord. When connected to a pulse generator, the ultra-thin electrodes start sending small electrical currents to the spinal cord, which disrupt pain signals.
Understanding the neural computations of pain will help us
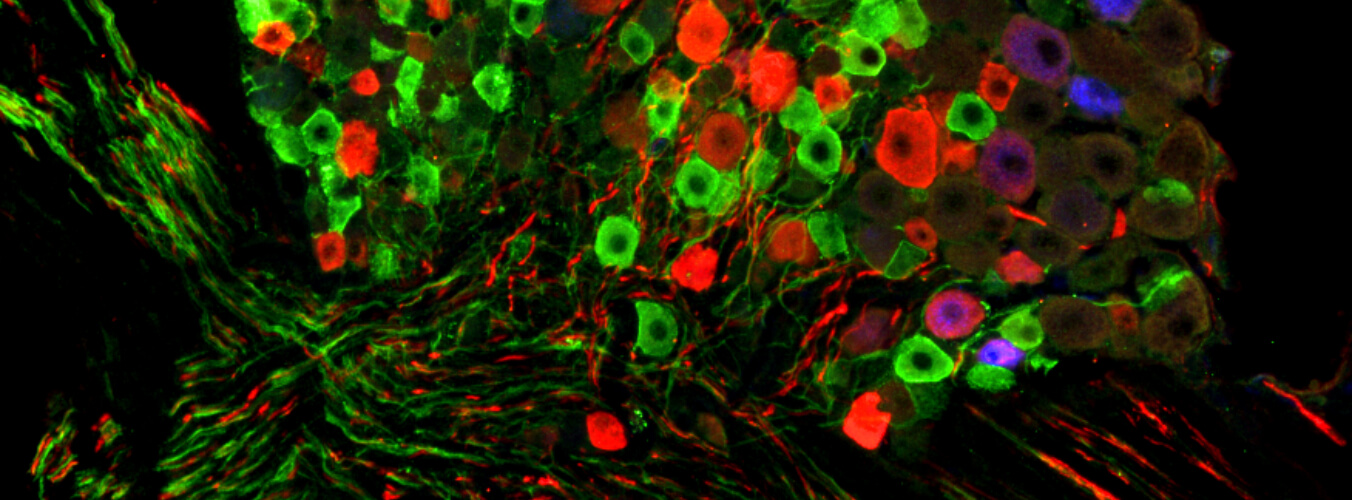
There are unresolved questions that urgently require answers to treat pain effectively, a crucial one being how the feeling of pain arises from brain activity. Researchers are using computational models of pain consider how the brain processes noxious information and allow mapping of neural circuits and networks to cognition and behaviour. Understanding neural computations of pain dynamics is essential to improve the prevention, treatment and management of chronic pain.
Further support would be profoundly useful in many different areas which include:
- Developing our interdisciplinary research programmes in pain research
- Funding specific postgraduate programmes in pain research (PhD and Masters level).
You can watch a short documentary that considers whether robots should feel pain in Pain in the Machine (filmed in 2016) and Gut Reaction, which illustrates how clinicians and scientists are working to improve the lives of those living with bowel pain (filmed in 2019).